- Topics
- Webinars
- Products & Services
Welcome To Biggest Online compliance Platform By LOCGFX Pvt. Ltd.
Healthcare
This webinar includes all the new changes to the discharge planning standards that became effective November 29, 2019, and published in the February 21, 2020 manual. It is anticipated CMS will publish revised interpretive guidelines and survey procedures to match the new regulations in 2021. These apply to all hospitals, and for the first time will apply to critical access hospitals.
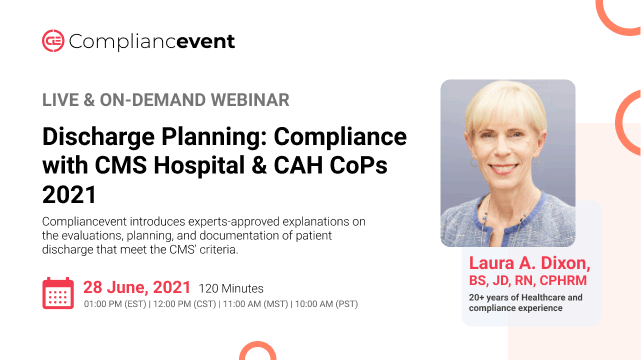
Compliancevent introduces experts-approved explanations on the evaluations, planning, and documentation of patient discharge that meet the CMS' criteria.
-CMS issues revised hospital & CAH Discharge Planning requirements
-How this will impact the discharge planning worksheet which will be amended
-Discharge planning process and required planning
-Identification of patients in need of discharge planning
-Evaluation of discharge planning
-RN, social worker, or qualified person to develop evaluation
-Timely evaluation
-Discussion of evaluation with patient or individual acting on their behalf
-Discharge evaluation must be in the medical record
-Documentation of the discharge process
-Discharge plan
-Physician request for discharge planning
-Implementation of the patient’s discharge plan
-Reassessment of the discharge plan
-Freedom of choice for LTC, LTCH, home health agencies, and inpatient rehab
-Document list to provide (except CAHs)
-Transfer or referral
-Detailed discussion on the CMS Discharge Planning Worksheet
-Overview of the discharge planning process, evaluation, and requirements
-Documentation of the discharge process
-Patient rights in relation to discharge planning
-To thoroughly discuss the CMS' revised discharge planning requirements that apply to all hospitals and critical access hospitals
-To recall patients and physicians can request a discharge planning evaluation
-To learn that information about the hospitalization must be provided to the physician or provider before the first post-hospital visit
-To describe that the patient has a right to get medical records timely including a copy of their discharge plan
-Transitional care nurses
-RN discharge planners
-Social workers
-Billing Office Directors
-Physicians
-All staff nurses who discharge patients in a hospital setting
-Nurse educators
-Health information directors
-Chief nursing officers
-Chief Operating Officers
-ED nurses
-Physicians
-Patient Safety Officers
-Discharge planners
-Nurse managers
-Staff nurses
-PI directors
-Chief medical officers
-Risk managers
-Social workers
-Physician advisors
-Regulatory officers
-All nurses with direct patient care
-Compliance officers
-UR nurses
-Joint Commission Coordinators
-Chief Operating Officers
-Chief executive Officers
-Hospital committee members who redesign the discharge process to prevent unnecessary readmissions

Laura A. Dixon served as the Director, Facility Patient Safety and Risk Management and Operations for COPIC from 2014 to 2020. In her role, Ms. Dixon provided patient safety and risk management consultation and training to facilities, practitioners, and staff in multiple states. Such services included the creation of and presentations on risk management topics, assessment of healthcare facilities; and development of programs and compilation of reference materials that complement physician-oriented products.
Ms. Dixon has more than twenty years of clinical experience in acute care facilities, including critical care, coronary care, peri-operative services, and pain management. Prior to joining COPIC, she served as the Director, Western Region, Patient Safety and Risk Management for The Doctors Company, Napa, California. In this capacity, she provided patient safety and risk management consultation to the physicians and staff for the western United States.
Ms. Dixon’s legal experience includes medical malpractice defense and representation of nurses before the Colorado Board of Nursing.
As a registered nurse and attorney, Laura holds a Bachelor of Science degree from Regis University, RECEP of Denver, a Doctor of Jurisprudence degree from Drake University College of Law, Des Moines, Iowa, and a Registered Nurse Diploma from Saint Luke’s School Professional Nursing, Cedar Rapids, Iowa. She is licensed to practice law in Colorado and California.
Compliancevent Webinar Certification - Compliancevent rewards you with Compliancevent Achievement Certification for unlocking and attending this webinar. It is to acknowledge your participation in this training session and to add more to your professional score.
Compliancevent Courses and Webinars or any Education published "Articles & Materials" strictly follows the standards and guidelines of the Professional Credit / CEU Providers and Well Researched before publishment.
Compliancevent doesn't support any Fake - News, Articles, or Compliance updates; Our Industry Experts are highly verified and recognized, and their Pre-publishment is verified via our experts and fact-checkers.
Sign up now on compliancevent.net. Visit compliancevent.net/webinar to discover a wide range of webinars from industry specialists. Tick on either ‘live webinar’ or ‘on-demand’, and simply click on ‘buy now’ to get enrolled.
You can refer compliancevent to anyone in your social circle. Explore your industry with your colleagues by getting them signed up on compliancevent.net today!
Go for the topic of your keen interest on compliancevent.net. Tick on ‘live webinar’ and get enrolled! Easy registration, transparent transaction.
You can request for an on-demand webinar that records the live webinar for you. After the webinar ends, you will have full access to the webinar’s recording. You can also explore compliancevent offline to order your webinar DVDs, flash drives and transcripts.
If you can’t attend the live webinar, simply go for the ‘on-demand webinar’ for the same price! Now, the live webinar recording will be saved in a cloud storage for you to access anytime from anywhere.
compliancevent offers both hard and soft copies of the webinars. It contains all the highlights as well as comprehensive descriptions of the webinar, so you never miss out a single detail.
After attending the live webinar, your certificate will be emailed to you. You can download it and add more charm to your professional score.
At the end of each webinar, you have the opportunity to interact with your industry experts, where you will get answers to all your queries.
Can’t attend the live webinar? compliancevent has got you covered! You can always switch to the on-demand webinar from your portal. You can also get your hands on the webinar’s DVD/flash drive and transcript. So order them now!
compliancevent brings a variety of options for offline learning. Order your DVDs, flash drives or transcripts now to have a lifetime access to compliancevent webinars. You can also go for on-demand recordings. Download and watch it anytime from anywhere in the world!